In this interview, Professor Iruka N. Okeke, a long-time champion of typhoid control, speaks with SADE OGUNTOLA on reasons Nigeria should deploy the typhoid vaccine to prevent infection, whether drug-sensitive or resistant.
HOW is your drug discovery approach helping to combat childhood diarrhoea?
Our drug discovery research is still at its very early stage. We are interested in targeting bacteria that cause childhood diarrhoea, which are neglected because those who discovered the drugs don’t see diarrhoea in infants as a viable market. So, we are trying to see whether we can take on these bacteria, understand how they make children sick and then also understand how to block the sicknesses that they cause.
We want to understand what the principal causes of diarrhoea are, including collecting stool specimens from children with diarrhoea and from healthy one for comparison and to identify specific components that cause illness. Major cases of diarrhoea in our setting are preventable if people have access to good water, if the sewage doesn’t get into drinking water and if our food is not faecal contaminated.
At the moment, one vaccine is already available to protect children from diarrhoea, that is the rotavirus vaccine. It’s recommended for mothers to get for their babies. After the rotavirus vaccine, there is no other vaccine for the germs that cause childhood diarrhoea, but there are about 100 different germs that children need to be protected from. Obviously, we can’t give a baby 100 vaccine to cover all of these germs. If we know what the four most common types are, a combined vaccine can be made for those four and then you will get rid of 80 percent of the diarrhoeal disease. So, we are trying to understand the most prevalent germs that cause diarrhoea. This also feeds into our drug discovery work, in terms of identifying germs that we should prioritise for drug discovery to treat infected children.
What is antimicrobial resistance, how bad is it in Nigeria?
Antimicrobials are very powerful and useful medicines. They are taken by people who have infections; most of us have taken an antibiotic or an antimalarial some time in our life. All of these are antimicrobials; they worked really well against germs that cause disease in the past. If you had an infection in the past and you took something like Ampicillin, Tetracycline and or Septrin®, you would recover in three to four days and be fine.
Unfortunately, the germs that these antibiotics used to kill are now becoming resistant to them. That means, if you have what used to be a very simple infection that could be very easily treated, and by chance you are prescribed an antibiotic but doesn’t not get well, you would then be prescribed second course of medicine, which still may not work. And the longer these germs stay in the body, the more the chance they will lead to a worse illness or even death. So, antimicrobial resistance is essentially the germs learning to be able to fight back against the antimicrobials that we previously used to treat infections. The first approach to getting around antimicrobial resistance is just to invent more drugs. Unfortunately, the germs are becoming resistant faster than we can create drugs. It takes 20 to 25 years to create a new drug, whereas the bacteria can sometimes acquire resistance in just a few days. So we need to think carefully about how to prevent antimicrobial resistance.
Is the resistance occurring in all available antimicrobials or a selected few?
Resistance has been reported on all antimicrobials that have been used in clinics. You would have heard that Alexander Fleming discovered penicillin. In his lifetime, he saw resistance to penicillin. So it’s actually quite a common phenomenon. Unfortunately, the drugs that are most affected are the older drugs that tend to be cheaper; cheap drugs that you can take orally so you don’t have to go to a hospital for injections. Of course, resistance to the newer and more expensive drugs is less common, but it is still there. The implications are quite dire for all, because that then means patients and the society would have to pay more to get treated when sick. Sometimes, you will hear someone went to the hospital and the antibiotics needed are the very expensive ones. It is because the germs causing that infection are resistant to the cheaper antibiotics.
The other thing is the actions of a few that promote resistance, leading to problems for many. It is not the human being that become resistant, it is the germ. So someone can become infected with a germ that is resistant while not having done anything anything wrong. The implications are societal, though individuals are contributing to the problem.
Talking about antimicrobial resistance, what are the diseases being affected more in Nigeria?
It is a whole range of diseases. For example, bloodstream infections called bacteraemia, typhoid and malaria. In the past, we used chloroquine, a very cheap drug, to treat malaria. Now, nobody uses chloroquine because resistance has taken over. We now use the artemisinin-based combinations that are much more expensive. Tuberculosis is another disease that antimicrobial resistance has made very difficult to treat.
The Nigeria Centre for Disease Control (NCDC), the agency responsible for the control of diseases in the country, has several surveillance systems. Some of them are disease specific, such as the cholera surveillance system. NCDC’s antimicrobial resistance surveillance looks at all bacteria that can cause severe infections. When hospitals around the country perform tests on patients and identify resistant germs, they report such to NCDC. The agency validates their results and collates the information, so we know how much resistance is present in the country and also the types of resistance.
Unfortunately, resistance by common diseases like typhoid to the first-line drugs that can be given orally is quite common. For example, more than half the bacterial isolated from typhoid are resistant to what used to be the best drug for treating it – Ampicillin, Septrin® and the likes. There are second-line drugs that can be used like injectable-antibiotics. For now, these work in Nigeria but there are other settings where they don’t work. We are already seeing low levels of resistance to the second-line drugs too. There’s a chance that in the future, things will get worse.
How about cholera, it keeps re-emerging every year?
Cholera is actually a devastating disease; it kills very quickly. But cholera resistance is less of an issue today because the approach for treating cholera does not rely entirely on antibiotics. The reason people die so quickly from cholera is because they lose their body water so quickly. The approach now is that as soon as you find patients with cholera, quickly rehydrate them and then let their immune systems help deal with the infection. There is also a cholera vaccine. When an outbreak occurs, the most effective thing is to vaccinate people around the individual who has cholera so that they too do not get cholera.
Talking about the severe typhoid in Africa project, what are some of your findings?
The project is a very large collaborative one that is essentially trying to understand the burden of typhoid in Ibadan and other parts of Africa. Our finding is that after malaria, typhoid is actually the most common cause of serious fever. This is something that wasn’t known. Often, people with fever are told that they have typhoid. But it is not necessarily true because the test is done to detect typhoid, but it is not very reliable. The Widal test is unlike the blood culture test that is more precise, although it is more expensive and takes a long time. When we started the surveillance using the blood culture, it was thought that we would not find much typhoid. But we actually found a lot; it is enough to be able to say that typhoid is a huge problem in Ibadan. After malaria, typhoid is the most common cause of febrile disease in this setting.
So, how huge is the burden of typhoid, especially now that it is common to hear people say they have both malaria and typhoid?
Yes, lay people often say that but I’m not sure all those cases are typhoid, because they only had a widal test. Many of those widal tested individuals don’t have typhoid. Using blood culture, we have been able to show that typhoid is quite common, particularly in young children up until school age. A lot of them get severe typhoid; severe typhoid can cause intestinal perforation. If one doesn’t get to hospital fast enough for surgery if there is intestinal perforation, one could pass away. As you know, surgery is quite expensive and you need specialist surgeons to be able to do it. Unfortunately, some of the germs that cause typhoid are resistant to antibiotics. So it’s important to continue surveillance so that we know which antibiotics work and which ones don’t. When a patient does have typhoid, we will then know which antibiotics are better to use.
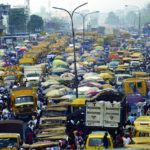
Another thing that we observed in our research on typhoid and its spread in Ibadan is the environment. We have seen that many households in Ibadan, for example, do not have good quality water. The water is contaminated with microorganisms. This is part of why water-borne diseases, including typhoid, can spread very easily. People without a water purifying system at home should consider boiling the water they drink to be sure that they do not get typhoid. To boil water with fuel or gas is very expensive, but managing typhoid is much more expensive.
There is an effective vaccine for typhoid and it has been deployed in other countries. Now that we have evidence that when people suspect typhoid, a good proportion of them do have typhoid, Nigeria needs to adopt the vaccine. We have justification for saying that though the vaccine is a bit costly, it’s something that is worth it in the country. It is still cheaper to vaccinate people than to treat intestinal perforation and severe typhoid.
Protection from two doses of the vaccine will last about five to six years. This is particularly important because most people found to have severe typhoid or dying from it were between ages two and 10. If we give a two-year-old Typhoid Conjugate vaccine, it will cover him or her over the period of highest risk of having severe typhoid. If individuals get typhoid later in life, it is less likely to be severe. Before resistance to the second-line drugs that are still useful in Nigeria appears, it will be important to deploy the vaccine. This will prevent people from getting typhoid infection in the first place, whether sensitive or resistant.
You are also working on neglected enteric bacteria that are able to cause potentially bloodstream infections. Are there other findings from your work that you will like to share as well?
In addition to finding that typhoid is a very common cause of fever, there are other bacteria that cause diseases very similar to typhoid that are not very common elsewhere but are common in Nigeria. Also, based on the work we are doing, we found for example that school-age children also come down with Salmonella infections other than typhoid. Non-typhoidal Salmonella is almost as common as typhoid in Nigeria. Beside this, we’re finding newborns with bloodstream infection called newborn sepsis due to some common bacteria. In all, we are pushing vaccine developers to prioritise development of vaccines against those conditions now that we know the types of organisms causing the infections.
As a basic scientist, what are the challenges in prioritising research for health?
A major challenge is the need for strong infrastructure. Getting constant electricity to run scientific equipment in Nigeria is hard. Electricity is also becoming more expensive. The other issue is that most young scientists in our setting that do a lot of the work I have described are underpaid and undervalued. They don’t see a future for themselves in Nigeria, though they hold our future. They are less motivated and they might leave to work in more conducive settings. This would be a lost investment for us, because research is expensive and the training is expensive too. Science in the country is underfunded. We need to be putting our money where our mouth is. Nigeria needs to invest in its own research so that it priority can be given to diseases that affect us most.