As the number of COVID-19 cases declines, another health crisis is already on the rampage. FUNMILAYO AREMU examines the monkeypox virus, its causes, treatment, and preventive methods.
Goodbye, COVID, hello, monkeypox!”; “Pandemic, season two, episode one – the return of masks”; “Chickenpox, we know, measles, we know, but what’s monkeypox again?.” These are some of the concerns expressed by Nigerians on their social media platforms as news of yet another viral disease emerged in 42 countries worldwide.
Just as there appeared to be some respite following the sudden drop in new cases of COVID-19, a new wave of viral infection known as monkeypox (MKPV) has emerged across the globe.
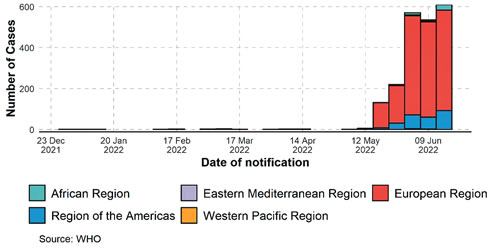
According to the Centre for Disease Control and Prevention, 3308 cases of monkeypox have been reported globally, with European countries leading the way with the most cases. In Nigeria, 41 cases and one death have been reported as of Tuesday, June 21, by the Nigeria Centre for Disease Control (NCDC).
According to the World Health Organisation, monkeypox is a viral zoonosis, meaning that it is a virus transmitted to humans from animals.
Sunday Tribune spoke with some medical experts to shed more light on the disease. A clinical Microbiologist at the Federal Medical Centre, Abuja, Dr NkolikaUwaezuoke, said despite being zoonotic it is however, not a deadly disease, though it should be given proper attention.
“Monkeypox belongs to the orthomyxovirus genus, which includes other diseases you’ve probably heard of, such as smallpox, vaccinia, and cowpox, as well as several other animal-related pox viruses.
“It is endemic in West Africa and Central Africa. The virus has two distinct strains; the West African strain is the one we have here in Nigeria and is typically associated with less severe illness. Then we have the Congo Basin or the Central African strain which is more virulent and causes more severe infections,” she explained.
Dr Chukwuemeka Anya, a public health official at the FMC Abuja, while explaining the latest health emergency to Sunday Tribune described the symptoms of monkeypox, as being similar to those of malaria.
“Many of them are constitutional symptoms, which means they are similar to what you would experience if you had malaria. There is fever, joint pain, muscle pain, weakness, vomiting, lymph node swelling, and then rashes appear, looking generally like chicken pox, some just appearing, some already containing fluid, some just appearing without fluid, some have burst, and others are already healing; so you see them at various stages. That is how it appears. monkeypox’s incubation period is 5 to 21 days; typically, one to two weeks after exposure, the person develops a rash that lasts three weeks,” he explained.
Speaking further on possible symptoms of monkeypox, Dr Uwaezuoke explained that “The infection is usually mild, and many patients with monkeypox are asymptomatic, which means they don’t have symptoms. Those who do have symptoms will typically have a fever, headache, muscle ache, backache, and swollen lymph nodes, a condition known as lymphadenopathy. The patient may also have chills and, in some cases, a sore throat and cough as part of the initial symptoms.
“After about the days of the initial fever, headache, and swollen lymph nodes, patients begin to see the appearance of a typical monkeypox rash. This rash usually appears on the face, but it can also appear on other parts of the body, such as the genitals and perianal area, which is the area surrounding the anus. Typically, the legion in monkeypox will go through several stages before drying up, forming a crust, and eventually falling off; this could take up to a month. It is important to note that patients are infectious from the time the first symptoms appear until the rash falls off. The time between the initial symptom and the rash falling off can be two to four weeks.”
How it is transmitted
Dr Anya is of the opinion that those whose livelihood depend on selling of bush meat have to be careful as the virus can be transmitted during the process of preparing it for sale. He added that being in contact with infected people and animals can also spread the virus. Connoisseurs of bush meat also have to be avoid their favourite pass time for the time being.
“Most of the transmission occurs through close body contact with infected individuals. Contact with infected animals is another way. When you handle animals, particularly those that eat bush meat, transmission can occur during the preparation process. Some people keep them as pets; however, it is mostly from bush meat. That is usually when the virus spreads.
“The problem with this particular outbreak is that there has been a lot of community spread; person to person spread. This time, the animals have played very little role in the spread of this particular outbreak. Most of the spread has been among humans and that is what makes it frightening. So, people that have no contact whatsoever with animals had contracted it. With viruses, you’re more scared, not about what is happening at the moment, but what could happen.
“If a virus has low virulence, that is, it doesn’t kill a lot of people, mutate or combine with other viruses already in the body, we don’t know what it can produce. If it now produces something that spreads rapidly and causes possible death, it can produce a different organism different from the two organisms that combined to form it. That is usually the problem with viruses. That is what I think is causing the panic,” he opined.
Dr Uwaezuoke also elucidated the origin and first instance where the virus was discovered. “The first case of monkeypox was discovered in laboratory monkeys in 1958, followed by the first human case in the Democratic Republic of the Congo in 1970.
“The next case was in 2003 when it was imported into the United States in a shipment of exotic African rats, which passed it on to American prairie dogs, who then passed it on to humans, which is how it came about in America. It used to be endemic in West and Central Africa alone, but the current outbreak has been discovered in European countries that have never reported it,” she said.
She further stated that sexual contact with an infected person, as well as touching items like beddings, clothing, and other personal effects of an infected person, as well as direct contact with the rash or body fluid from such rashes on an infected person’s body, can all result in virus transmission.
“Recently, it was discovered in the Western world that one thing that new cases have in common is that they are men who have sex with men or men who are gay. Avoid contact with animals that may be infected with the virus or with dead animals whose cause of death is unknown.
“This virus is easy to spread. Close, prolonged face-to-face contact is one way to spread the virus. It is less transmittable than other viruses such as Ebola and Lassa fever. When you come into contact with an animal that has the virus, it will have to scratch or bite you, or if you are exposed to the animal’s body fluid as you prepare its meat to eat,” she explained.
She also mentioned some animals to be on the lookout for, adding that animals that harbour the virus are referred to as reservoirs. They (the animals) are exotic pets such as the Gambian Giant rat, prairie dogs, squirrels, and monkeys.

Possible complications
When asked if the monkeypox virus could come with complications, Dr Uwaezuoke stated that while it is not a fatal disease, complications could occur.
“The majority of people will recover, but complications may arise. In areas where monkeypox is endemic, such as West and Central Africa, complications such as encephalitis (brain inflammation) can occur. It can also affect the patient’s eye, causing conjunctivitis, respiratory distress, secondary bacterial skin infection, and even pneumonia. Young children whose immune systems have not fully developed, and people who are immunocompromised (those with HIV, tuberculosis, cancers, or diabetes) are at risk of severe complications,” she said.
Treatment and precautionary measures
Many people wonder if the virus can be treated because it was discovered that viruses have no cure. Dr Uwaezuoke clarified that, while it is not a fatal disease, there are antiviral drugs that have been shown to treat viral illnesses such as monkeypox.
“Monkeypox is not a fatal disease,” she said, adding that “so far, we have lost one patient in Nigeria. In comparison to other illnesses such as COVID-19, it is not a fatal disease. However, public health attention is still required because you don’t want people spreading it; you must still educate people on how to prevent it.
“Milder cases will not require treatment, and if treatment is required, it will usually be supportive. The US Food and Drug Administration (FDA) has approved anti-viral agents that can be used to treat monkeypox. These medications were actually approved for the treatment of smallpox. Later, it was discovered that the agents were also effective in treating diseases caused by other orthopoxviruses, of which monkeypox is one. Anti-viral medications used to treat severe cases of monkeypox include Tecovirimat, Cidofovir, and Brincidofovir. Milder cases are self-limiting, which means they run their course and then disappear,” she said.
When asked if anti-viral drugs are widely available, she stated that “these drugs are new drugs and are not easily accessible for those with severe cases. In Nigeria, the strain is mild and self-limiting. I’m not sure if these drugs exist in Nigeria, but they are not easily accessible.”
Dr. Anya clarified that the virus is not lethal because the mortality rate is low; however, the disease is more severe in children.
“Previously, we had reports from previous outbreaks that had a 1 to 3 per cent mortality rate. Ordinarily, that is high, but this outbreak has not resulted in significant mortality. There had been over 2600 cases prior to the death that was recorded, but there had been no mortalities as of June. The mortality rate is very low. Children are more severely affected. Adults will recover,” he pointed out.
Both Dr. Anya and Dr.Uwaezuoke believe that avoiding body contact with infected people, sick or dead animals, or materials used by an infected person can help to slow the spread of the virus.
According to Dr.Uwaezuoke, people should “avoid becoming intimate with somebody who has a rash until the rash heals and a fresh layer of skin forms. The first step is to isolate an infected person from others; this breaks the chain of transmission. Hand hygiene is especially important for health care workers after coming into touch with an infectious person or animal.
“People should wash their hands frequently and apply alcohol-based hand drops, generally known as hand sanitiser. Healthcare staff must also take standard precautions. Another method of protection is vaccination with Jynneos, a live, attenuated, non-replicating smallpox and monkeypox vaccine.
Dr Anya on his part recommended that “When people are infected, they avoid close contact; frequent hand-washing would aid, especially after shaking so many people and without knowing who is already contaminated with what, including the usage of sanitisers.”
He also urged for increased awareness because many people, including some medical practitioners, are unaware of the disease and frequently dismiss it as chickenpox. Those who discover the rash should go to the nearest health care facility immediately.
“Our index of suspicion should be high; many people notice it but don’t know what it is. Greater awareness should be raised; many people identify it as chicken pox and that’s where it stops. Even medical colleagues will classify it as chickenpox. I can’t expect everyone who has a fever to come to the hospital; it wouldn’t be fair. However, when rashes appear, it is time for the person to come because the rashes can last for up to three weeks and are contagious.
“Please come to the hospital as soon as possible. Once the diagnosis is made, the person must isolate; in fact, the person must isolate until the results are available. The good news is, in Abuja, once you notify the State Epidemiology Unit about the patient, they come immediately and take samples, or you can take the samples and keep them, once they come, they take the samples, go and run it, and you usually get the results within 24 hours,” he explained.
Though the good news is that monkeypox is not fatal, yet self-isolation including other factors like right diagnosis and early presentation at the hospital by patients must be ensured and that is where the problem is, given the situation with our medical infrastructure. Until these are done promptly, cases might spiral due to community infection.
YOU SHOULD NOT MISS THESE FROM NIGERIAN TRIBUNE
Revealed! Details Of South-West APC Leaders Meeting With Presidential Aspirants
MORE revelations have emerged about Friday’s meeting held by South-West leaders of the All Progressives Congress (APC) with aspirants from the zone, whose main objective, was on how to avert a crisis that will create a fractured party as it prepares for primary on May 30 and 31, Sunday Tribune has reliably gathered…
Continuous Voters Registration: Bauchi declares Monday public holiday
Supreme Court Has Cleared Civil Servants To Participate In Politics, Falana Tells FG
Continuous Voters Registration: Bauchi declares Monday public holiday
NIGERIAN workers are constitutionally-free to participate in politics, lawyer, Mr Femi Falana has said. He was responding to the warning from the central government to civil servants to stay off politics…
Battle For New Alaafin Begins As Ruling Houses Insist On Producing Next Oba
WATCH TOP VIDEOS FROM NIGERIAN TRIBUNE TV
- Let’s Talk About SELF-AWARENESS
- Is Your Confidence Mistaken for Pride? Let’s talk about it
- Is Etiquette About Perfection…Or Just Not Being Rude?
- Top Psychologist Reveal 3 Signs You’re Struggling With Imposter Syndrome
- Do You Pick Up Work-Related Calls at Midnight or Never? Let’s Talk About Boundaries